Armor Correctional Health Services Lawsuit: Inmate Healthcare Failures, Legal Battles, and What These Cases Reveal About U.S. Prison Reform
The Armor Correctional Health Services lawsuit has become a defining example of how inmate healthcare neglect, underfunded medical systems, and weak oversight have created a nationwide crisis inside U.S. prisons. As correctional facilities continue to outsource medical care to private providers, concerns surrounding improper treatment, delayed response, and prison medical malpractice have grown louder—placing Armor at the center of national scrutiny.
Yet, this legal battle is not just about one company. It reflects deeper systemic issues that compromise Eighth Amendment inmate rights, raising questions about how the U.S. correctional healthcare system has allowed severe neglect to go unchecked for years.
This article examines the origins of the lawsuits, the most troubling allegations, and the high-profile cases that exposed widespread failures in inmate care—while also highlighting what these legal battles reveal about the urgent need for correctional healthcare reform across the country.
Why the Armor Lawsuit Matters Now
For years, the U.S. prison healthcare system has struggled with chronic understaffing, insufficient funding, and inconsistent oversight. Inmates—who rely entirely on prison medical teams—often report long delays, untreated illnesses, ignored emergencies, and inadequate mental health support. These failures create life-threatening situations that would be unacceptable in any other healthcare environment.
Armor Correctional Health Services, once a major medical provider in jails and prisons across multiple states, has faced mounting lawsuits accusing the company of severe inmate healthcare neglect. These cases allege delayed treatment, ignored symptoms, medication mismanagement, and even preventable inmate deaths. As a result, Armor has become a symbol of a broader, nationwide failure in correctional medicine.
These lawsuits expose a pattern of systemic neglect that goes beyond individual mistakes. Instead, they highlight deep structural problems—poor monitoring, inadequate training, and profit-driven decisions—that demand urgent reform.
Who Is Armor Correctional Health Services?
Armor Correctional Health Services (often referred to simply as “Armor”) is a private contractor that has provided medical, mental health, and dental services to inmates in correctional facilities across the United States. Their services included:
- Routine medical check-ups
- Chronic illness management
- Emergency response
- Mental health treatment
- Medication handling and distribution
Armor previously operated in jails and prisons in states such as Florida, New York, Wisconsin, Oklahoma, and Nevada, among others. Over time, the company entered dozens of contracts with counties and state facilities—but many of these partnerships later became controversial.
History of Contracts and Controversies
Armor once positioned itself as a cost-effective healthcare provider for overcrowded jails. However, as lawsuits accumulated, allegations of inadequate staffing, cost-cutting, and improper medical practices surfaced. Multiple counties later declined to renew contracts due to safety concerns, audit findings, and legal risks.
Many of the lawsuits filed today stem from incidents that occurred during Armor’s years of operation in major facilities like New York’s Nassau County Jail, Milwaukee County Jail in Wisconsin, and others.
| State | Key Issues & Contract Status |
| Florida | Multiple lawsuits filed for medical neglect. |
| Wisconsin | High-profile death investigation at Milwaukee County Jail. |
| New York | Lost contract after audits revealed severe deficiencies. |
| Oklahoma | Complaints of delayed medical care and medication issues. |
| Nevada | Reports of understaffing and critical delays. |
How the Armor Correctional Health Services Lawsuit Began
The rise of the Armor Correctional Health Services lawsuit was not the result of one event—it was the culmination of years of complaints, investigations, and preventable tragedies inside facilities they served.
Timeline of Events
- Early Complaints (Late 2000s–2012):
Families and inmates first reported issues such as ignored symptoms, worsening illnesses, and medication lapses. - Internal Audits (2013–2015):
Several counties commissioned audits, uncovering understaffing, poor documentation, and repeated protocol violations. - Whistleblower Revelations (2015–2016):
Former employees reported systemic issues—untrained staff, pressure to reduce medical costs, and lack of proper oversight. - High-Profile Deaths and Media Coverage (2016–2020):
When multiple inmates died allegedly due to delayed or denied care, media investigations amplified public outrage. - Lawsuits & Contract Terminations (2017–Present):
Dozens of lawsuits were filed nationwide, prompting counties to end long-term partnerships with Armor.
Systemic Patterns Identified
Rather than isolated incidents, lawsuits portrayed:
- Chronic understaffing
- Deliberate delays in treatment
- Ignoring urgent symptoms
- Poor emergency response systems
- Medical decisions influenced by budget constraints
These patterns set the foundation for the legal battles Armor still faces today.
The Core Allegations Against Armor (Detailed Analysis)
The Armor Correctional Health Services lawsuit centers around four major categories of inmate healthcare failures.
1. Medical Neglect & Delayed Care
One of the strongest allegations is that Armor routinely failed to provide timely medical treatment to inmates experiencing serious symptoms. Examples include:
- Inmates waiting hours—or days—for evaluation despite reporting chest pain, infections, or chronic illness flare-ups
- Triage failures where critical symptoms were downgraded or ignored
- Staff shortages leading to long delays in assessments
Deliberate or reckless delays violate Eighth Amendment inmate rights, which require prisons to provide adequate medical care and protect inmates from cruel and unusual punishment.
2. Failure in Emergency Response
Multiple lawsuits argue that Armor medical staff did not treat urgent medical events—such as cardiac distress, seizures, diabetic crises, or breathing difficulties—as true emergencies.
Specific failures included:
- Ignoring repeated requests for help
- Not calling external emergency services on time
- Misinterpreting serious symptoms as “behavioral issues”
- Allowing inmates to deteriorate for hours before responding
Medical experts reviewing these incidents concluded that emergency protocols commonly used in hospitals and clinics were not followed inside jails.
3. Mental Health Care Failures
Mental health is a crucial part of correctional health services, yet lawsuits reveal striking deficiencies:
- Inmates with diagnosed mental illnesses were left untreated
- Lack of suicide-prevention monitoring
- Inadequate mental health evaluations during intake
- Over-reliance on solitary confinement rather than treatment
Some tragic cases involved inmates harming themselves after repeated warnings were ignored.
4. Improper Medication & Lack of Equipment
Armor has also faced accusations of:
- Failing to administer essential medications on schedule
- Running out of critical drugs
- Mismanaging prescriptions for chronic diseases
- Using outdated or insufficient medical equipment
- Skipping diagnostic tests due to cost
Such failures can rapidly worsen conditions like diabetes, asthma, or heart disease, turning manageable illnesses into life-threatening emergencies.
High-Profile Cases: What Went Wrong (with Specifics)
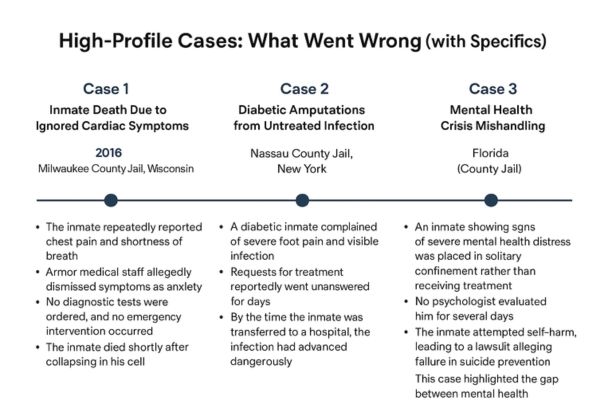
Case 1: Inmate Death Due to Ignored Cardiac Symptoms
Year: 2016
Location: Milwaukee County Jail, Wisconsin
Inmate: Michael Madden
Sequence of Events: Michael Madden, 29, collapsed in the jail after repeatedly reporting severe chest pain and breathing difficulties. Despite his visible distress and known heart condition, Armor medical staff allegedly failed to intervene or send him to a hospital. Witnesses stated that instead of receiving emergency care, he was told to “stop faking.”
Findings & Outcome: Madden died of infective endocarditis (a heart infection). His death—along with the dehydration death of inmate Terrill Thomas in the same facility—sparked a massive outcry. The county eventually paid a significant settlement, and prosecutors filed criminal charges against Armor staff for falsifying medical records.
Case 2: Fatal Medical Neglect & Contract Termination
Location: Nassau County Jail, New York
Inmate: John Gleeson
What Happened: John Gleeson, 40, suffered from angioedema, a condition that causes dangerous swelling. Despite evident swelling in his throat and difficulty breathing, Armor staff allegedly failed to send him to the hospital. He died of asphyxiation (choking) in his cell.
Lawsuit Outcome: The New York State Commission of Correction found Armor’s care to be “incompetent and deficient.” This case, combined with reports of other untreated conditions, led to the New York Attorney General suing Armor. The company ultimately paid a $350,000 settlement, agreed to a three-year ban on bidding for contracts in New York, and was forced out of the Nassau County facility.
Case 3: Mental Health Crisis & Starvation
Location: Broward County Jail, Florida
Inmate: William Burrell
Overview: William Burrell, a mentally ill inmate, stopped eating while in custody. Despite Armor staff documenting his rapid weight loss and deterioration, a federal lawsuit alleged they failed to intervene or hospitalize him due to “profit-driven” policies that discouraged off-site transfers.
Outcome: Burrell starved to death in his cell. His case became a central pillar in lawsuits accusing Armor of systemic “deliberate indifference” to mental health needs. It highlighted the dangerous gap between required mental health standards and the actual practices in privatized correctional facilities.
What the Lawsuits Reveal: Systemic Problems in U.S. Prison Healthcare
The Armor lawsuits do more than highlight company failures—they expose widespread issues embedded in correctional healthcare nationwide.
1. Chronic Understaffing & Budget Cuts
Many facilities rely on minimal medical teams who struggle to manage large inmate populations. Understaffing leads to delays, missed diagnoses, and rushed evaluations.
2. Lack of Training
Reports show that:
- Nurses lacked emergency response training
- Mental health staff were insufficiently certified
- Correctional officers were unprepared to identify medical crises
3. Oversight Gaps
Weak monitoring allowed systemic problems to continue unchecked:
- Inconsistent audits
- Poor record-keeping
- Limited consequences for repeated violations
4. Profit-Driven Healthcare Models
Private healthcare providers often aim to reduce costs—sometimes at the expense of adequate treatment. Inmates suffer when budget cuts override medical standards.
Legal Consequences: Why These Cases Are Constitutional Violations
1. Understanding the Eighth Amendment
The Eighth Amendment prohibits cruel and unusual punishment — a standard interpreted by U.S. courts to require that prisons provide adequate medical care to inmates.
The landmark case Estelle v. Gamble (1976) established that “deliberate indifference to serious medical needs” is a constitutional violation.
This means correctional healthcare providers must:
- Respond promptly to medical complaints
- Follow standard medical practices
- Prevent unnecessary suffering
- Ensure vulnerable individuals (chronic illness, mental health risks) receive protective care
Any failure to meet these duties is not simply malpractice — it is a constitutional breach.
2. How Armor’s Practices Violated Constitutional Rights
Based on lawsuit records, media investigations, and court filings, Armor’s actions met multiple criteria for “deliberate indifference”:
- Ignoring repeated complaints of chest pain, high fever, infections
- Failing to follow emergency protocols
- Allowing known chronic diseases to deteriorate
- Not administering life-saving medications on time
- Leaving mentally ill inmates unsupervised, resulting in self-harm or suicide
- Cutting staff or leaving shifts uncovered despite known facility needs
These patterns show more than isolated errors — they represent systemic disregard for inmate health.
3. Potential Criminal Liability or Federal Oversight
While most prison healthcare lawsuits result in civil penalties, legal experts note that:
- Federal intervention under the Department of Justice (DOJ) is possible if constitutional breaches are severe enough.
- Criminal liability could be considered in cases involving falsified medical records, intentional withholding of care, or reckless disregard for life.
- State-level bans on future contracts often follow high-profile cases, which Armor has already faced in some jurisdictions.
If more cases emerge, Armor could face deeper federal scrutiny similar to past prison healthcare crackdowns.
Regulatory Failures and Why Oversight Needs Reform
Current Laws vs. Enforcement Gaps
Although prisons must comply with constitutional medical standards, there is no unified national oversight system. Most monitoring is left to:
- State correctional agencies
- Local sheriffs
- Contract auditors
The problem? Enforcement is inconsistent and often underfunded.
What Independent Audits Revealed
Audits from several states reveal recurring issues:
- Staffing below contracted levels
- Missing medical documentation
- Improper triage procedures
- Medication shortages
- Failure to meet chronic care standards
In some cases, audits revealed that warning signs of inmate deterioration were documented but ignored.
Calls From Civil Rights Groups & Watchdogs
Organizations like the ACLU, Prison Policy Initiative, and Human Rights Defense Center argue that:
- Privatized healthcare companies prioritize profit over patient care
- Independent medical oversight is urgently needed
- States must enforce severe penalties for non-compliance
- Transparency in inmate medical records should be mandatory
Policy Changes Being Demanded
Advocates are pushing for:
- Annual federal audits of prison healthcare
- Public reporting of inmate health outcomes
- Whistleblower protections
- Mandatory minimum staffing levels
Financial Impact on Armor: Settlements, Penalties & Lost Contracts
Specific Lawsuit Costs
Public records show:
- Multi-million dollar wrongful death settlements
- Legal fees from ongoing class-action lawsuits
- Penalties for contract violations
How Lawsuits Hurt Future Bids
Several counties and states have terminated or refused to renew Armor’s contracts due to:
- High-profile inmate deaths
- Audit failures
- Public pressure from activists and media
Many municipalities now prefer providers with transparent systems and modern medical tracking.
Financial Performance Decline
As lawsuits increased, Armor experienced:
- Loss of major revenue streams
- Stricter contract conditions
- Lower competitive standing during bids
How These Lawsuits Affect Taxpayers
Ultimately, taxpayers bear the cost when:
- Lawsuit settlements are paid by county governments
- Prisons must find emergency replacement providers
- Delayed healthcare leads to more expensive treatments
The financial ripple effects make prison healthcare reform not only a moral issue — but an economic one.
The Future of Prison Healthcare: What Needs to Change
To prevent future tragedies, experts recommend major reforms focusing on accountability, technology, and oversight.
1. Mandatory Medical Staff Training
Regular training on:
- Emergency response: Including cardiac events and trauma care protocols.
- Chronic disease management: Standardizing care for conditions like diabetes and heart disease.
- Mental health crisis intervention: Ensuring staff can identify and manage acute psychological distress.
- Constitutional responsibilities: Educating staff on the legal requirement to avoid deliberate indifference.
2. Technology-Based Monitoring Systems
Facilities should adopt modern technology to reduce errors and increase transparency:
- Electronic Medical Records (EMR): To ensure comprehensive, shareable, and trackable inmate health histories.
- Automated medication reminders: To prevent the deadly errors associated with medication mismanagement.
- Digital triage systems: To standardize the initial assessment of medical complaints.
3. Third-Party Independent Oversight
Independent oversight bodies can break the cycle of self-monitoring by local authorities:
- Conduct surprise inspections and independent assessments.
- Audit medical charts and protocols for compliance.
- Review critical incidents and publish public reports on outcomes.
4. Federal vs. State Accountability Reforms
Experts suggest:
- Establishing national standards for correctional care that apply universally.
- Federal monitoring of high-risk facilities with histories of violations.
- Funding incentives for compliant prisons and severe penalties for non-compliance.
5. Changes Advocates Are Pushing For
Advocates want policy changes that prioritize health over cost:
- Transparency in healthcare contracts.
- Staffing ratios tied to population size.
- Dedicated mental health crisis units inside facilities, separate from solitary confinement.
What Inmates Need to Know About Their Rights
Even inside a correctional facility, inmates have legal protections guaranteed by the Constitution.
Legal Rights Under the Eighth Amendment
Inmates have the right to:
- Access medical care
- Receive timely emergency treatment
- Get medication for chronic illnesses
- Be protected from medical neglect
- Receive mental health services
What Qualifies as Medical Neglect
Neglect may include:
- Ignored medical complaints or requests for help.
- Delayed or denied treatment for serious conditions.
- Lack of follow-up for diagnosed conditions.
- Missing or improperly supervised medications.
- Unsafe withdrawal supervision.
Steps Families Can Take
Families worried about an inmate’s health should:
- Request medical welfare checks from the facility administration.
- Document all communications, including dates, times, and staff names.
- Request medical records (where legally allowed).
- Contact advocacy groups for support (e.g., ACLU or local prison watchdog organizations).
When to Consult a Prison Rights Attorney
A lawyer should be contacted when:
- An inmate’s health is rapidly deteriorating.
- There is proof of ignored medical requests or symptoms.
- A serious injury or death has occurred due to lack of care.
- Medical records appear incomplete or altered.
Conclusion
The Armor Correctional Health Services lawsuits expose deep-rooted failures in the U.S. correctional healthcare system. These are not isolated tragedies — they are symptoms of a larger national problem involving understaffing, poor oversight, and profit-driven decision-making.
By understanding these cases, analyzing constitutional violations, and pushing for meaningful oversight reforms, the public, lawmakers, and advocates can work toward a safer, more humane prison system.
Legal action plays a critical role in holding providers accountable — and in revealing the urgent need for nationwide correctional healthcare reform.
FAQs
1. What is the Armor Correctional Health Services lawsuit about?
The lawsuits involve claims of medical neglect, delayed treatment, and constitutional violations under the Eighth Amendment.
2. What rights do inmates have when it comes to medical care?
Inmates have the right to adequate medical treatment and protection from neglect under constitutional standards.
3. What are examples of medical neglect in prisons?
Ignored symptoms, lack of emergency response, missing medications, untreated injuries, and ignored mental health crises.
4. How many lawsuits has Armor faced?
Armor has faced multiple lawsuits across several states, including wrongful death suits, class-action claims, and contract violation cases.
5. Can families sue for inmate medical negligence?
Yes. Families can file wrongful death suits, negligence claims, or constitutional violation lawsuits depending on the situation.
6. What reforms are being proposed for prison healthcare?
Proposed reforms include federal oversight, mandatory training, EMR systems, independent audits, and stronger staffing standards.



